- Haemolytic disease of the fetus / newborn (HDFN) is caused by maternal antibodies against fetal red cell antigens.
- IgG antibodies can cross the placenta and cause haemolysis.
- Incidence of clinically-significant antibodies in pregnancy: 0.3-1%.
- Greatest risk with anti-D, anti-c and anti-K (and all other Kell system antigens, e.g. anti-k, -Kpa, -Kpb, -Jsa, -Jsb) .
- ABO incompatibility may also cause haemolysis.
- Maternal blood group should be checked at booking and 28 weeks to determine ABO/Rh status and screen for clinically significant red cell antibodies (e.g. anti-D, -c, -K)
- If detected, further testing should be done to assess the likelihood of these causing HDFN
- Antibody titres should also be measured once every four weeks until 28 weeks, then once every 2 weeks till delivery
- Moderate risk of HDFN: anti-D levels 4-15 IU/ml, anti-c 7.5-20 IU/ml
- Severe risk of HDFN: anti-D levels of >15 IU/ml, anti-c >20 IU/ml
- If the mother has clinically-significant antibodies, then the father and fetus should be tested to ascertain the risk of the fetus carrying the relevant antigen
- Free fetal DNA can be extracted from the maternal circulation from 16 weeks
- If the fetus is antigen positive and the mother has clinically-significant antibodies, then the pregnancy must be monitored closely. Middle cerebral artery peak systolic velocity is a non-invasive and sensitive way of detecting fetal anaemia.


0 x
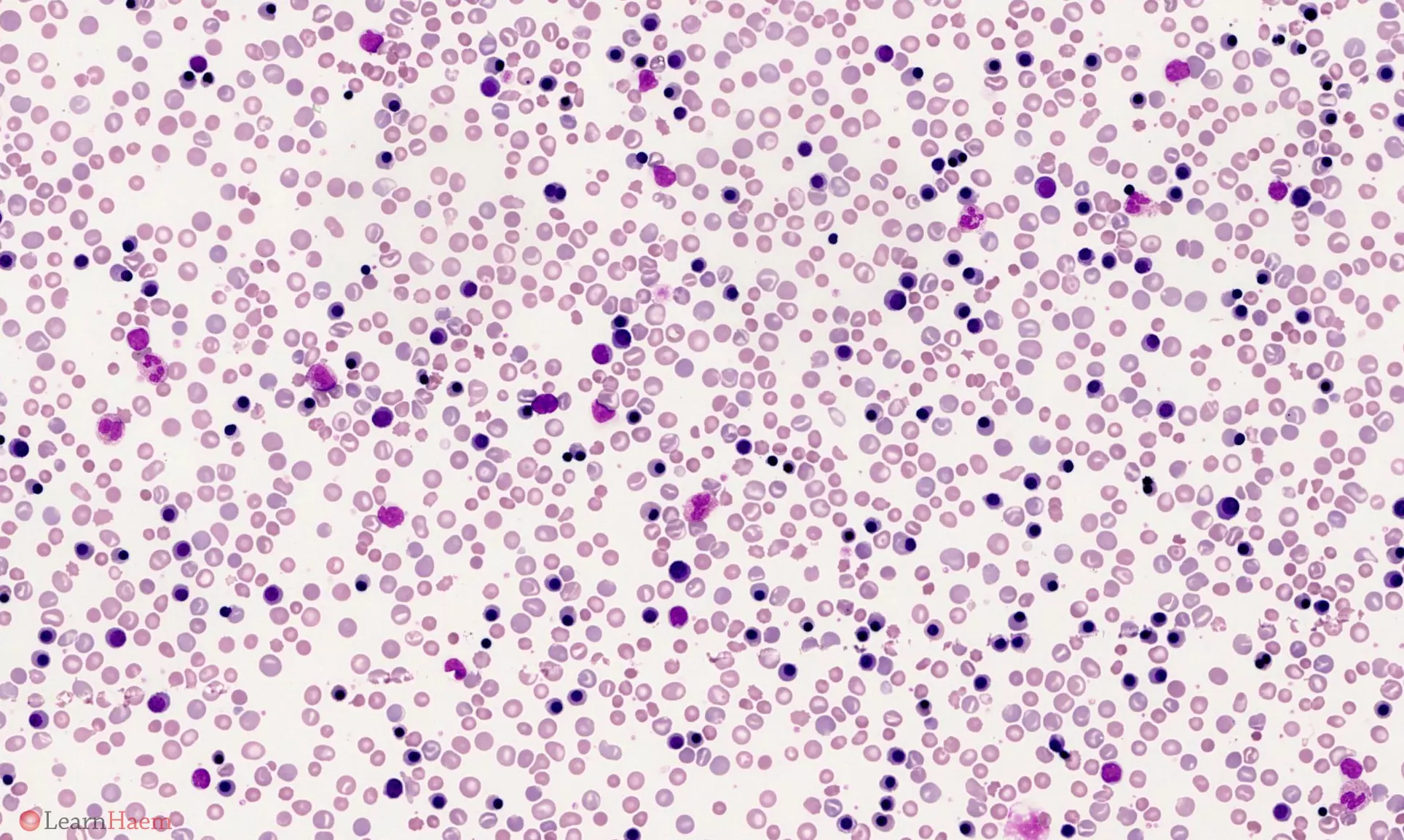
Blood film features:
- Spherocytes
- Polychromasia
- Circulating nucleated red blood cells
- Polychromasia and circulating nRBCs may be absent in Kell haemolytic disease of the newborn because of associated marrow suppression.
Differential diagnosis:
- Hereditary spherocytosis
Other resources:
- BCSH Guideline: Anti-D Immunoglobulin for Prevention of HDFN (2014)
- RCOG Guideline: Red Cell Antibodies in Pregnancy (2014)
- BCSH Guideline: Blood Grouping and RBC Antibody Testing in Pregnancy (2016)
- ASH Image Bank: RhD HDN
- ASH Image Bank: Erythroblastosis Fetalis
- HDFN (Transfusion Medicine Reviews 2016)

Leave A Comment