Acute myeloblastic leukemia with maturation is characterized by the presence of ≥ 20% blasts in the bone marrow or peripheral blood with evidence of maturation.
Diagnostic Criteria (WHO 2016)
- ≥20% blasts in the bone marrow or peripheral blood
- Evidence of maturation – ≥10% of maturing cells of granulocytic lineage
- Monocyte lineage <20% of bone marrow cells


0 x
Blood Film Features:
- Leucocytosis with myeloblast
- Thrombocytopenia


0 x
Bone Marrow Features:
- Bone marrow is usually hypercellular
- Myeloblast: commonly with auer rods and azurophilic granules
- Monocyte lineage < 20% of bone marrow cells


0 x
Blood film from a patient with acute myeloid leukaemia with maturation and a t(8;21) translocation. Note the presence of blasts with auer rods and maturing myeloid cells in the peripheral blood.


0 x
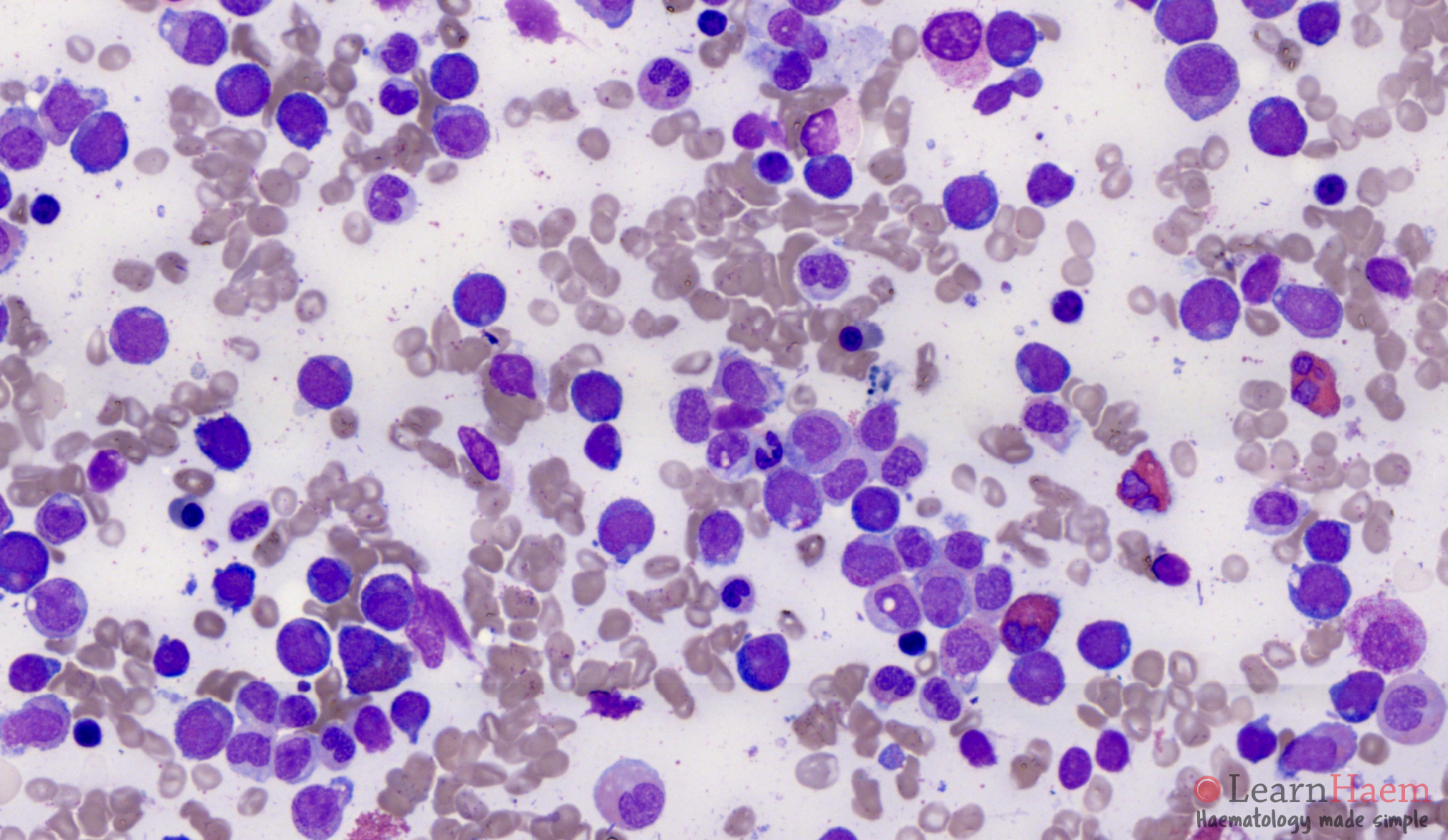
Bone marrow aspirate from a patient with AML t(8;21). Note the numerous eosinophilic myelocytes. This is AML M2-Eo (M2 with eosinophilia). The blasts have a peri-nuclear hoff, basophilic cytoplasm and azurophilic granules, which is characteristic of AML t(8;21). The blasts are expected to be dimly positive for CD19 on flow cytometry.
Other features to look for:
- Variable degrees of dysplasia
- Increased basophils and mast cells
- Eosinophil precursors – suggestive of M2Eo
- Blasts with a perinuclear hof, abundant basophilic cytoplasm with azurophilic granules – suggestive of acute myeloid leukaemia with t(8;21)(q22;q22.1)

Fascinating.