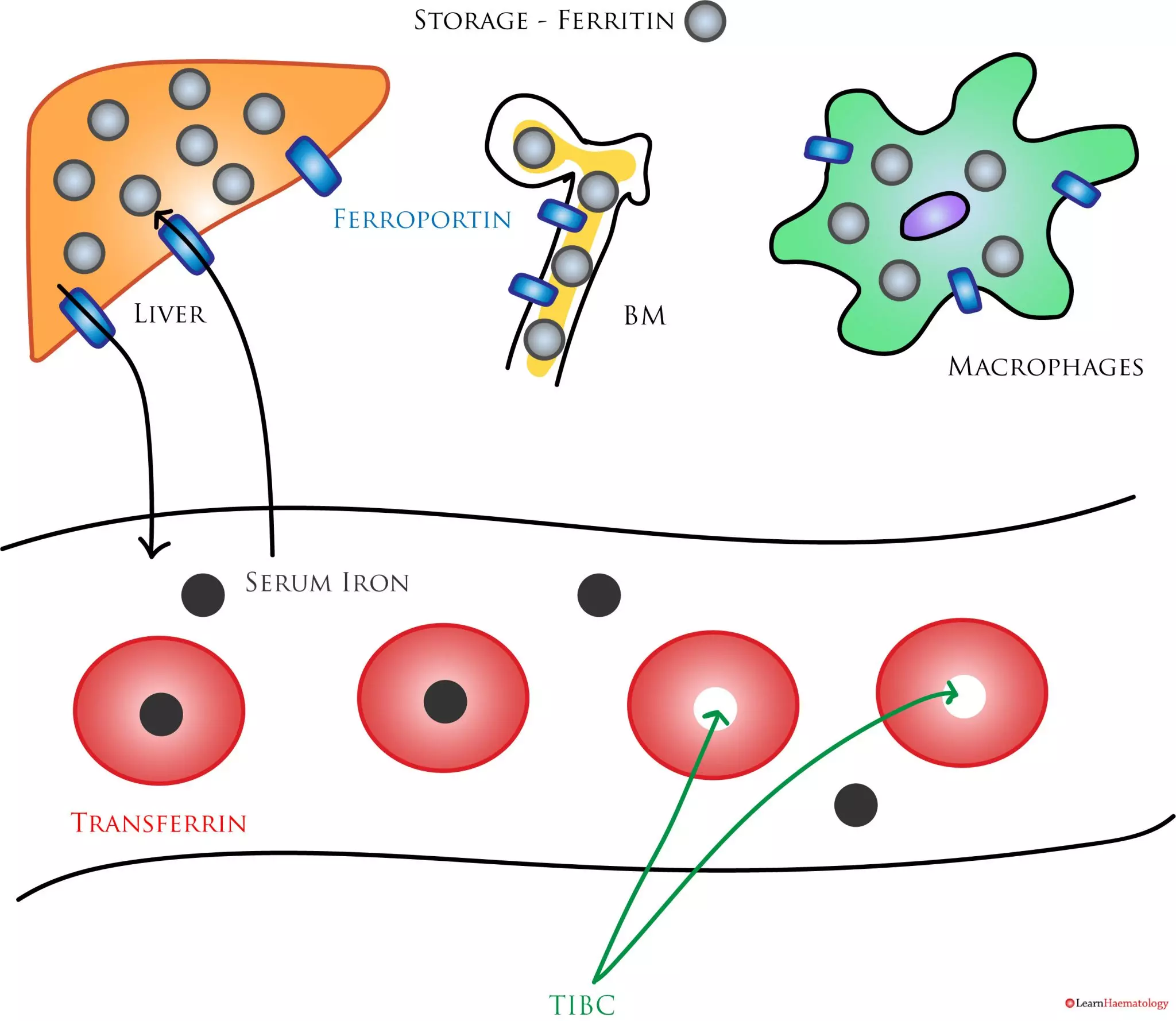
Iron studies are one of the most commonly ordered laboratory tests. The figure below shows a schematic representation of the a few common laboratory tests of iron balance, and how they relate to iron storage and transport.
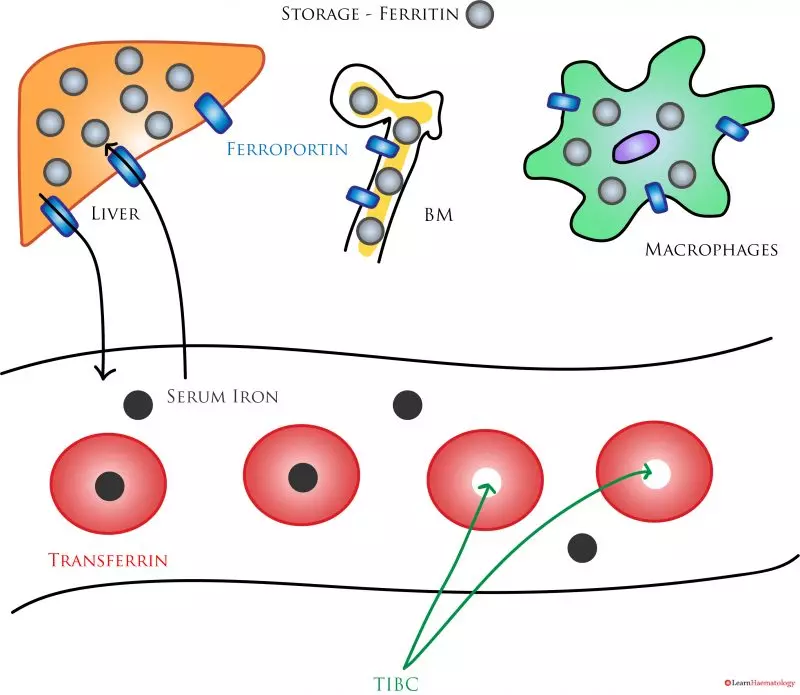
Laboratory Measures of Iron Balance. Ferritin (light grey circle) is the main storage protein. Iron enters and exits the storage compartments via ferroportin (blue rectangle). In the blood, iron may be free (black circle), or bound to transferrin (red doughnut). The total iron binding capacity (TIBC) is the amount of available iron binding sites. The transferrin saturation is calculated by dividing the serum iron by the TIBC.
Serum iron is a measure of circulating iron, most of which is bound to transferrin. The serum iron level is low in iron deficiency and inflammatory anaemia because it depends on efficient recycling of iron through macrophages and the bone marrow. In iron deficiency, there is insufficient iron for iron recycling, while in inflammatory anaemia, increased hepcidin levels result in iron trapping in macrophages.
Transferrin is the main iron transport protein; its synthesis is inversely proportional to body iron stores. Hence, levels increase in iron deficiency to facilitate iron absorption. Transferrin levels are often low in inflammatory anaemia as transferrin expression is negatively affected by cytokines.
Ferritin is the main iron storage protein. The normal range is 15 – 300 µg/dL. The sensitivity and specificity of the test vary depending on cut-off levels used to define iron deficiency; at a cut-off level of 15µg/L, the test is highly specific for iron deficiency, but lacks sensitivity. At a cur-off level of 100µg/L, the sensitivity increases to 94%, at the expense of specificity (71%). Ferritin is a positive acute phase reactant; levels increase in inflammation. In addition, levels in inflammatory anaemia may also be high because of ferritin secretion by iron-retaining macrophages.
The total iron binding capacity (TIBC) reflects the available iron binding sites on transferrin. It requires the measurement of serum iron and transferrin that is not bound to iron (i.e., the unbound iron binding capacity, UIBC). The TIBC is the sum of serum iron and the UIBC. TIBC and transferrin are essentially different measures of the same parameter. The TIBC is high in iron deficiency but low in inflammatory anaemia. The transferrin saturation is the ratio of serum iron to the TIBC, expressed as a percentage. Levels fall in both iron deficiency and inflammatory anaemia.
The table below summarises the changes in the various laboratory indicies in different disease states:
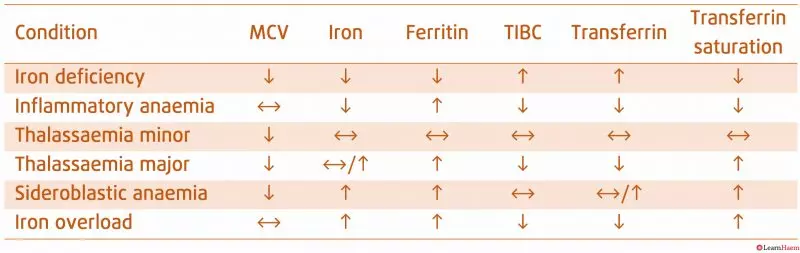
Iron Indices. Ferritin is the most specific marker of iron deficiency; its sensitivity is dependent on the cut-off value. A serum ferritin of <30µ/L is very sensitive for iron deficiency.

WHAT CAN YOU DO IF YOU HAVE HIGH IRON IN YOUR BLOOD STREAM
You should discuss this with you doctor. Elevated iron levels can be due to haemachromatosis, which can result in liver damage if untreated. Fortunately it is easy to treat and will not harm you if kept under control. Again, it is important to discuss this with your doctor.
Chris Holden
Medical Doctor, Tasmania, Australia.
I have slightly elevated serum iron and extremely high saturation, but low ferritin (31). I’m negative for hemochromatisis. None of my doctors know what to do. Everything else is normal, including hemocrit and hemoglobin. RBC on the low end of normal, RDW on the low end (cut-off) of normal. MVC and MCH are high. What testing should I ask for?
Thanks so much,
Jamie
I basically have the same issues as you. Did you get some answers since your post?
Did you ever get an answer or treatment for this? I have the same problem
Very good. Basic concepts are very clearly explained
The problem I have with the up/down/sideways arrow charts is that in real practice they often aren’t helpful.
For example the inpatient with colon cancer, high ferritin as an acute phase reactant, but there may be coexistent Fe deficiency–the TF sat is barely low, or low normal. What’s a useful cutoff there to decide if the patient would benefit from Fe infusion.
More information regarding test performance characteristics at different quantitative cutoffs (like you do for ferritin) would be helpful.
Can you go into more detail of what to look for with thalassemia. With iron 54 mcg/dL, IBC 241 mcg/dL, % sat of 22, transferrin 182 mg/dL, retic count 77,760 cells/uL and 1.8%, and ferritin 217 ng/mL, along with hgb that’s slightly low and MCV of 83.4, platelets of 428k, hct 36.7, I’m guess either a low grade inflammation? How would one detect recovering anemia or recently repleted anemia?
Hello
I am trying to work out the Mass Balance of where the Iron is in the Body:
Iron is present in Hemoglobin and Red Blood Cells
Iron is Transported via Transferin
Iron is stored in Ferritin
Therefore Total Iron Store in the Body = Free Iron in the Blood (Iron Serum) + Iron Stored in Ferritin + Iron Transported via Transferin+ Iron in Red Blood Cells + Iron in Hemoglobin
Is that Right?
Total Iron Store for Adult Males is 4 gms and Females 3.5 gms
Could you please provide the evidence behind this
“The sensitivity and specificity of the test vary depending on cut-off levels used to define iron deficiency; at a cut-off level of 15µg/L, the test is highly specific for iron deficiency, but lacks sensitivity. At a cur-off level of 100µg/L, the sensitivity increases to 94%, at the expense of specificity (71%).”
Please interpret these results. Getting nowhere with Docs, i.e., “everything is fine” yet I’m weak and lost about 70% of my hair. I’m a female at 67+ yrs.
Test results in last year:
TIBC: 556, 508
Ferritin: 40, 32.1
Iron: 103, 117
Transferrin: 393, 363
Saturation: 19, 23
Results in past few years:
TIBC: 454. 459
Ferritin: 57.1, 42, 47, 44
Iron: 58, 44,
Transferrin:
Saturation: 13, 10
Did see info on this on stopping the thyroid madness website as caused by MTHFR or?? Also could be low B12 to use the iron, according to B12oils site, B12 needs B2 (it needs I,Se), so I try eating organic chicken liver(only thing available) or cod liver. My MCV is high in and if you have B12 defic and iron defic than it will balance some of lab results. Found the B12 lab is not very accurate (if have antibodies…) so an active B12 lab or/& mma urine lab (homocsyteine may be helpful)
I have been confused about iron studies. My patient has ferritin 8 (Low based on WHO criteria), but high iron 191 and high transferrin saturation. Patient feels well. She does carry homozygous H63D mutation, but this mutation is not usually associated with iron overload picture. Based on her ferritin, she is even on the iron deficient side. I cannot explain why iron and transferrin saturation are high.
Hi
Have you been lucky to find out the cause? This is exactly what I have. High iron 203 , high saturation (66), but low ferritin of 16! What am I supposed to do?
Thank you
It’ s the same for me!! Have either of you been able to figure this out? I’m going nuts here, I want to feel better and stop loosing hair.
Is it possible to interpret the same iron studies in someone who has already been transfused RBCs for anaemia?
Yes it is – if they are still iron deficient, it likely means that they were iron deficient to begin with. However, if their iron studies are normal, it may be slightly confounded.
What does it mean when your transferin saturation (17%) is low and feritin normal 45ug/L? (Iron 13 umol/L). Patient experiences heavy periods and weakness/lethargy but more so during periods. Experiences significant hair loss.
Is it a cause for concern?
Great summary and very helpful table. Does this represent all possible known patterns? For example when one has elevated total serum Iron but low ferritin what condition does that indicate? It seems like a peculiar contradiction but there appear to be two other people inquiring about the exact same presentation in this comment thread. If this is a pattern that you are familiar with please elaborate. Thank you for your time.
I was hoping to have help deciphering my TIBC results.
I don’t eat much and may be anemic. Hair thinning and sometimes dizzy when standing up.
I have all the lab results that i can send.
I am not sure how versed my doctor is and would perfer to know the interpretation of results before my visit.
Great explanation, thank you
What about if your ferritin is low, transferritin is low and tibc is low??
All the Iron test are normal but ferritin is 650 and patient has Thalassemia Beta minor. How to reduce this ferritin level for this patient of mine. Phlebotomy and chelate tablets are not considered. did any one had such an experience in reducing ferritin level in a creative or unique way?
I have been receiving iron infusions for 12 years. I have iron deficiency without anaemia, although the 3 month wait for last infusion resulted in me becoming anaemic. I usually have an iron infusion once a year but ferritin is dropping quicker so last one was 6 months and now it’ only seems to have lasted 3 months. I’ve had camera tests and no cause found. Is it possible that there is no cause or have they just not found it yet? I’m 71. No other underlying conditions. I eat an iron rich diet but I can’t tollerate iron tablets.